What is it?
Chronic ankle instability is a condition where the structures responsible for the stability of the ankle have been compromised in some way. The ankle may feels as though it will give way or roll over during simple day to day activity where one would be expected to have otherwise good stability. For example, simply walking on the grass could be enough to destabilise someone who has chronic ankle instability. Ligaments, on the inside and outside of the ankle, and muscles work together to maintain the stability of the ankle joint. Instability may result from either weakness of the muscles or stretching of the ligaments, through injury or as part of a generalized laxity, or a combination of both.
How did I get it?
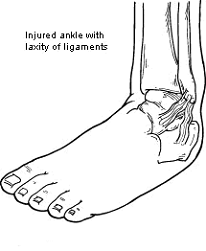 Commonly a severe ligament sprain or repeated ligament sprains over time are responsible for the instability and in most cases this involves the ligaments on the outside of the ankle. Instability may also result from a minor sprain where incomplete rehabilitation has occurred, as the muscles can be retrained to aid in the stability of the ankle. Generalised ligament laxity may also contribute significantly to any instability.
Commonly a severe ligament sprain or repeated ligament sprains over time are responsible for the instability and in most cases this involves the ligaments on the outside of the ankle. Instability may also result from a minor sprain where incomplete rehabilitation has occurred, as the muscles can be retrained to aid in the stability of the ankle. Generalised ligament laxity may also contribute significantly to any instability.
What does it feel like?
The most common sign is a feeling that the ankle is going to give way too easily. There may also be chronic inflammation and/or tenderness at the front, outside part of the ankle. Instability is commonly associated with a lack of range and stiffness when comparing to the unaffected ankle.
How is it diagnosed?
Patient history will generally provide a provisional diagnosis of instability. Ligament testing usually indicates an increase in the accessory (forward) movement of the talus bone within the mortise. MRI and ultrasound are useful for confirmation of complete ruptures and ligament tissue quality or attenuation.
How do I fix it?
- The first stage is to restore proper range of motion if this has been affected. Stretching may be helpful for muscular restricted range and physiotherapy for joint stiffness.
- Strengthening and proprioceptive exercises will help to restore the dynamic component of stability. Functional proprioceptive exercises need to be included before a return to sport.
- Ice over the tender area and anti-inflammatory medication will help keep swelling down and reduce pain.
Will I need surgery?
In some cases conservative therapy is not successful and surgery to tighten the ligament is required. The surgery consists of placing an anchor in the fibula bone and drawing the proximal end of the ligament toward the bone via a suture. The ligament will eventually attach to the fibula and restore normal function to the ankle.
How do I stop it coming back?
For those that choose surgery, a post operative protocol of strengthening and proprioceptive therapy should be enough to restore and maintain good control of the ankle joint.
If conservative measures are under taken then it depends on the mechanism for instability. Good tissue quality and minimal accessory movement will respond well to a similar program as the post operative protocol and require little revision. If there is significant ligament laxity then a comprehensive strengthening and proprioceptive exercise routine may need to be revisited from time to time to maintain good control.